Abstract
Introduction: Myeloproliferative neoplasms (MPNs) are clonal hematopoietic neoplasms and include polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF), etc., each with specific diagnostic criteria. Patients who display features compatible with MPN but do not meet the diagnostic criteria for a specific entity are commonly assigned a diagnosis of MPN, unclassifiable (MPN-U). JAK2, CALR, and MPL are well-known driver mutations in PV, ET, and PMF. With the advancement and application of next-generation sequencing (NGS), the molecular profiles of the above 3 well-defined MPNs have been extensively studied. However, the molecular profile of MPN-U remains ill-defined. In this study, we aimed to describe the clinical and molecular features of MPN-U in our institution and then compare these features between patients with and without JAK2, CALR, or MPL mutations to better understand the clinicopathologic characteristics and prognosis of MPN-U.
Method: The patients with a diagnosis of MPN-U and available NGS test results at our cancer center were identified and divided into two groups: cohort A) MPN-U with mutations in JAK2, CALR, or MPL, and cohort B) triple-negative. The patients' survival data, clinical parameters, bone marrow findings, and cytogenetics were collected for comparison. Baseline characteristics and somatic mutation distributions were compared using the chi-square test (categorical variables) and Wilcoxon rank sum test (continuous variables). Overall survival (OS) was calculated using the Kaplan-Meier method and compared using the log-rank test. A Cox proportional-hazards model was used to evaluate the association between OS and clinical factors.
Results: Out of 8285 patients in our institutional clinical molecular database which houses NGS, we identified and confirmed MPN-U diagnosis in 53 patients. Among this group, 39 patients harbored JAK2 (n=36), CALR (n=1), MPL (n=1), or JAK2 and CALR co-mutations (n=1) and were assigned to cohort A. The remaining 14 patients were triple-negative and assigned to cohort B.
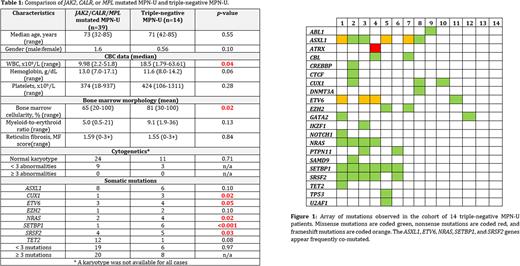
The triple-negative patients in cohort B had higher median WBC count (18.5 x 10 9/L vs 9.98 x 10 9/L, p=0.04) and bone marrow cellularity (81% vs 64%, p=0.02) (Table 1). The mutational profile of cohort B was enriched for CUX1, ETV6, NRAS, SETBP1, and SRSF2 mutations. ASXL1 and SETBP1 were the most frequently mutated genes in the triple-negative group, and were often co-mutated with ETV6, NRAS, and/or SRSF2 (Figure 1). TET2 mutations appeared more common in cohort A, but this finding was not statistically significant. There were no significant differences in the other parameters, including gender, bone marrow blast percentage, karyotype, hemoglobin concentration, platelet count, and bone marrow fibrosis.
Kaplan-Meier analysis demonstrated that the median OS time in cohorts A and B was not reached, and survival differences were not statistically significant (p-value 0.23). We used a Cox proportional-hazards model to evaluate the association between OS and clinical factors. Via backward elimination, we uncovered that high WBC count and low hemoglobin concentration were significantly associated with worse outcome (hazard ratios of 1.04 and 1.33, respectively, and p-values of 0.007 and 0.01).
Conclusion: In our small cohort, the patients with MPN-U who were triple-negative for JAK2,CALR, and MPL mutations had more frequent CUX1, ETV6, NRAS, SETBP1, and SRSF2 mutations. ASXL1 and SETBP1 were the most frequently mutated genes in the triple-negative group, and were often co-mutated with ETV6, NRAS, and/or SRSF2. In addition, triple-negative patients had higher WBC counts and higher bone marrow cellularity. A Cox proportional-hazards model identified high WBC count and low hemoglobin concentration as being significantly associated with a worse outcome. Kaplan-Meier analysis did not reveal a difference in OS between triple-negative and JAK2, CALR, or MPL mutated MPN-U. A larger cohort is needed to evaluate the survival outcome of these two distinct groups.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal